Planning Makes Safe Pregnancy Possible
Recent research from the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study supports the finding that with proper care and planning, people with epilepsy can have safe, healthy pregnancies and healthy babies.
However, pregnancy planning is critical for success. Research shows that different anti-seizure medications (ASMs) are associated with different levels of teratogenic risk. Consequently, for best outcomes, people with epilepsy need to start planning for pregnancy with their clinician 12 months in advance, as it can take 3-12 months to switch or adjust their ASM if they are on an ASM that has a higher level of teratogenic risk.
ASMs can also have interactions with different contraceptive methods. This should be taken into consideration when a patient enters child-bearing years. For more information on interactions between various ASMs and contraception, visit Contraception Options page.
Topics covered on this page include:
ASMs & Risks in Pregnancy
Several ASMs have been well studied in pregnancy, whereas many others still need more data. The best-studied outcomes are the risk of fetal malformations and the risk of adverse neurodevelopmental outcomes.
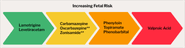
Fetal malformations and adverse neurodevelopmental outcomes with exposure to ASMs are relatively low compared to thalidomide, fetal alcohol exposure, etc. However, these outcomes vary significantly by ASM, with some having known elevated risk compared to others. See the figure below for information on the teratogenic risk profiles of ASMs.
** = Neurodevelopmental risks are not yet known
Risk stratification in medication choices based on all factors and available data can be summarized as follows:
- Lowest Risk: Lamotrigine or levetiracetam monotherapy
- Modestly Elevated Risk: Carbamazepine, oxcarbazepine, zonisamide*
- Moderately Elevated Risk: Phenytoin, phenobarbital, topiramate
- Highly Elevated Risk: Valproic acid. If it has to be used, it should be prescribed at the lowest effective dose. If possible, aim for doses of 500 to 600 mg/day (some patients can go as low as 250 mg/day)
- Unknown Risk: Other ASMs including, but not limited to, brivaracetam, cenobamate, eslicarbazapine, ethosuxamide, lacosamide, and perampanel
For more information on the specific risks for neurodevelopmental and fetal malformation, visit Child Development and ASMs page.
Cannabidiol & Marijuana (CBD & THC)
Use of marijuana, CBD or other THC products, or prescription cannabidiol (including Epidiolex®) is not recommended during pregnancy planning/pregnancy due to unknown effects on fetal development and probable adverse effects on neurodevelopment in utero. Even when from licensed dispensaries, these drugs may contain unknown levels of pesticides and fertilizers.
Switching ASMs & Pregnancy
Ideally, medication switching should occur well before pregnancy, not once a patient is already pregnant. Switching during pregnancy exposes the fetus to more than one medication and may increase the patient’s risk for seizures.
One exception is in the case of valproic acid, as this ASM has been found to be associated with the highest risk of malformations and adverse neurocognitive outcomes. If a patient is taking valproic acid, it is important to counsel them on risks related to switching medications before and during pregnancy (including increased seizures). Data show that valproic acid is the highest-risk ASM when it comes to the development of a fetus and that the negative effects on fetal brain development are probably the greatest in the third trimester. Also, consider the impact of valproic acid on other comorbidities.
For more information on switching a patient’s ASM (including in the case of valproic acid), visit the Switching ASMs page.
Guide Your Patients
Information about ASMs and pregnancy can be complicated for patients. Take the time to walk them through their different options.
Patients of childbearing age who are actively trying to conceive, and those who are in their childbearing years who are not yet considering pregnancy, should consider ASM teratogenic risk as part of the decision criteria for ASM selection. Emphasize to your patients that they should not stop taking their ASM medication before or during pregnancy due to fear or perceived risk.
*malformation data suggests low risk for malformations, no meaningful neurodevelopmental data
Reviewed by: Page Pennell, MD FAES, August 2023